Hepatitis
Hepatitis is an inflammatory condition of the liver that can result from different causes, including viral infections, excessive alcohol consumption, certain medications, and autoimmune diseases.
The term “hepatitis” broadly refers to liver inflammation, but it is most commonly associated with viral hepatitis, caused by distinct viruses known as hepatitis A, B, C, D, and E. These viruses differ in their modes of transmission, severity, and long-term effects on liver health.
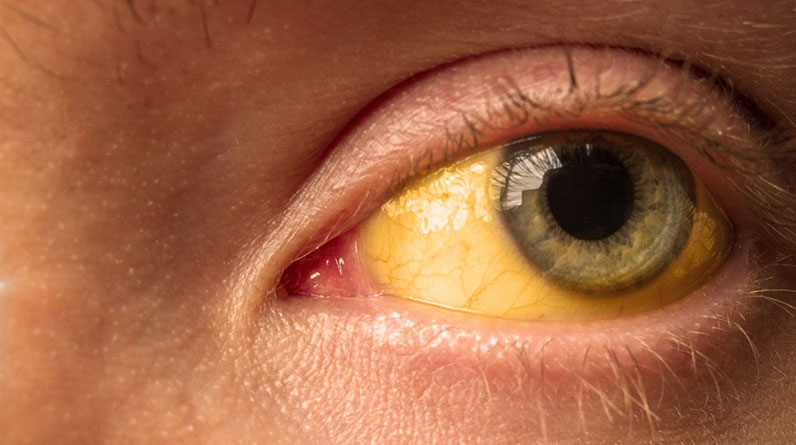
Symptoms of hepatitis are varied depending on the type and stage of the disease. In the acute phase, common symptoms include fatigue, flu-like symptoms, dark urine, pale stool, abdominal pain, loss of appetite, and jaundice (yellowing of the skin and eyes).
In what follows, we will talk about the different types of hepatitis, their causes, symptoms, and potential complications, offering a comprehensive overview to enhance awareness and guide effective management.
Types of Hepatitis
By studying the different types of hepatitis, their modes of transmission, and associated symptoms, practical methods are identified for effective prevention, early diagnosis, and appropriate treatment.
Hepatitis A
Hepatitis A is primarily transmitted through the ingestion of food or water contaminated with the feces of an infected person. It can also spread through close personal contact with an infected individual, though this is much less common.
The symptoms of hepatitis A usually appear suddenly and can include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, pale stool, joint pain, and jaundice. Most people recover fully within a few weeks to months, and the infection does not typically lead to chronic liver disease.
Hepatitis B
Hepatitis B is spread through contact with infectious body fluids, such as blood, semen, and vaginal fluids. Common modes of transmission include unprotected sex, sharing needles or syringes, and from mother to child during childbirth. It can also be transmitted through needlestick injuries and other exposures in healthcare settings.
Acute hepatitis B may present with symptoms similar to hepatitis A, including fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, pale stool, and jaundice. Some individuals, particularly young children, may be asymptomatic. Chronic hepatitis B can lead to long-term liver issues, including cirrhosis and liver cancer, often without noticeable symptoms for years.
Hepatitis C
Hepatitis C is primarily transmitted through blood-to-blood contact. This includes sharing needles or other equipment to inject drugs, receiving contaminated blood transfusions, or in some cases, organ transplants. Hepatitis C can can also be transmitted through sexual contact or from mother to child during childbirth, but these modes of transmission are less common.
Many people with acute hepatitis C are asymptomatic or have mild symptoms, such as fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, and jaundice. Chronic hepatitis C often remains asymptomatic for decades but can lead to significant liver damage, including cirrhosis and liver cancer, as the virus slowly progresses.
Hepatitis D
Hepatitis D, also known as delta hepatitis, only occurs in individuals already infected with hepatitis B, as it requires the hepatitis B virus to replicate. It is transmitted through contact with infectious body fluids, similar to hepatitis B, including through intravenous drug use and from mother to child during childbirth.
The symptoms of hepatitis D are similar to those of hepatitis B but can be more severe. These include fatigue, joint pain, abdominal pain, dark urine, nausea, vomiting, and jaundice. Coinfection with hepatitis B and D often leads to more rapid progression of liver disease, including a higher risk of cirrhosis and liver cancer.
Hepatitis E
Hepatitis E is primarily transmitted through the ingestion of fecal-contaminated water. It is common in regions with poor sanitation. Transmission through undercooked or raw meat from infected animals has also been reported.
Symptoms of hepatitis E are similar to those of hepatitis A and include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, dark urine, pale stool, joint pain, and jaundice. While most people recover fully, hepatitis E can be severe in pregnant women, leading to higher rates of liver failure and mortality.
Treatment, Management, and Prevention
The treatment, management, and prevention of hepatitis encompass a range of strategies tailored to the specific type of hepatitis virus involved. These strategies include antiviral medications, lifestyle changes, regular monitoring, vaccination, and adherence to safe practices.
Antiviral Medication
- Hepatitis B: Chronic hepatitis B can be treated with antiviral medications such as tenofovir, entecavir, and pegylated interferon. These drugs help reduce viral load, decrease liver inflammation, and prevent the progression to cirrhosis and liver cancer.
- Hepatitis C: The advent of direct-acting antiviral (DAA) medications has radically changed the treatment of hepatitis C. Drugs like sofosbuvir, ledipasvir, and glecaprevir have high cure rates, typically achieved within 8 to 12 weeks of treatment. These medications target specific stages of the virus’s lifecycle, effectively eliminating it from the body.
- Hepatitis D: Treatment options for hepatitis D are limited, but pegylated interferon may help suppress viral replication. Ongoing research is directed to more effective therapies.
- Hepatitis A and E: There are no specific antiviral treatments for hepatitis A and E. Treatment focuses on supportive care, including rest, hydration, and avoiding liver stressors.
Lifestyle Changes
- Diet and Nutrition: A balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports liver health. Patients should avoid alcohol and limit the intake of fatty, sugary, and processed foods.
- Exercise: Regular physical activity helps maintain a healthy weight and supports overall liver function. Exercise also reduces the risk of non-alcoholic fatty liver disease (NAFLD), which can exacerbate hepatitis.
- Avoiding Hepatotoxic Substances: Patients should avoid alcohol and be cautious with medications, supplements, and herbal remedies that can harm the liver.
Regular Monitoring
- Liver Function Tests: Regular blood tests to monitor liver enzymes (ALT, AST) and bilirubin levels help assess liver health and the effectiveness of treatment.
- Viral Load Testing: Measuring the amount of virus in the blood helps evaluate the response to antiviral therapy and the risk of disease progression.
- Imaging Studies: Ultrasound, CT scans, and MRI can detect liver damage, cirrhosis, and liver cancer early, facilitating timely intervention.
Vaccination
- Hepatitis A and B: Vaccines are available for hepatitis A and B. The hepatitis A vaccine is recommended for travelers to endemic areas, those who have unprotected sex, and individuals with chronic liver disease. The hepatitis B vaccine is part of routine immunization schedules for infants and is also recommended for unvaccinated adults at risk, such as healthcare workers and those with multiple sexual partners.
- Hepatitis C, D, and E: Currently, there are no vaccines for hepatitis C, D, and E. Preventive measures focus on reducing transmission risks.
Safe Practices
- Hygiene and Sanitation: Proper handwashing, safe food handling, and access to clean water are crucial to preventing hepatitis A and E, which are often spread through contaminated food and water.
- Safe Sex Practices: Using condoms and reducing the number of sexual partners can lower the risk of hepatitis B and C transmission.
- Safe Needle Use: Avoiding the sharing of needles and ensuring safe practices in medical and tattoo settings are vital to preventing hepatitis B and C. Needle exchange programs and safe injection sites can help reduce transmission among intravenous drug users.
- Blood Screening: Rigorous screening of blood donations helps prevent the transmission of hepatitis B and C through transfusions.
The comprehensive management of hepatitis involves a combination of antiviral medications, lifestyle modifications, regular medical monitoring, vaccinations, and adherence to safe practices.
These measures help to control the spread of the virus, decrease liver damage, and improve the quality of life for individuals affected by hepatitis. Early intervention and continued vigilance are the best ways to manage this diverse group of liver diseases effectively.