Liver Transplant Considerations
Liver transplantation is a life-saving procedure indicated for individuals with severe liver dysfunction that cannot be managed through other medical treatments.
The populations that typically require a liver transplant include those suffering from chronic liver diseases, acute liver failure, and certain genetic conditions.
Chronic Liver Diseases
Chronic liver diseases are the most common reason for liver transplantation. These conditions cause progressive damage to the liver over time, ultimately leading to end-stage liver disease or cirrhosis.
The most frequent causes of chronic liver diseases include hepatitis B and C, non-alcoholic fatty liver disease (NAFLD), and alcoholic liver disease. Hepatitis C, in particular, has been a leading indication for liver transplants, although recent advances in antiviral treatments have significantly reduced this need.
Patients with cirrhosis experience complications such as severe jaundice, fluid accumulation in the abdomen (ascites), bleeding varices, and hepatic encephalopathy, which are significant indicators of the need for a transplant.
Acute Liver Failure
Acute liver failure, also known as fulminant hepatic failure, is a rapidly progressing condition in which the liver suddenly loses its ability to function.
This condition can be caused by various factors, including viral hepatitis (especially hepatitis A and B), drug-induced liver injury (notably from acetaminophen overdose), and toxin exposure.
Acute liver failure requires immediate medical attention and, if not managed in a timely manner, can be fatal. For individuals who do not respond to medical treatment, a liver transplant becomes the only viable option.
Genetic Conditions
Certain genetic conditions can also lead to the need for a liver transplant. These conditions, present from birth or developing early in life, result in metabolic disorders that cause significant liver damage.
Examples include Wilson’s disease, which causes copper accumulation in the liver, and alpha-1 antitrypsin deficiency, a disorder affecting a protein that protects the lungs and liver. These genetic conditions often lead to liver failure or significant liver damage that necessitates a transplant for long-term survival and improved quality of life.
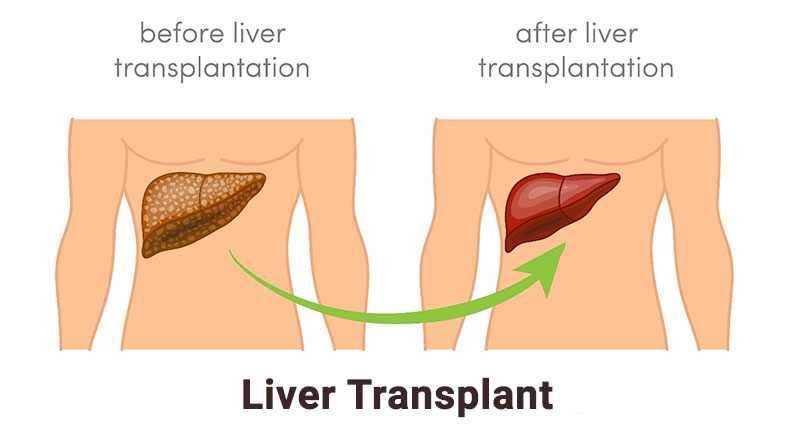
The Liver Transplant Process
Liver transplantation is a complex and meticulously coordinated process that involves several critical stages: evaluation, matching and allocation, and the surgery itself. Each stage is specifically important to ensure the success of the transplant and the long-term health of the recipient.
Evaluation Stage
During this stage, potential candidates undergo comprehensive medical, psychological, and social assessments to determine their suitability for a transplant. This evaluation includes tests and consultations with a multidisciplinary team of healthcare professionals, including hepatologists, transplant surgeons, cardiologists, and psychologists.
Medical tests typically involve blood tests, imaging studies (such as CT scans or MRIs), and liver function tests to assess the severity of liver disease and overall health. The team also evaluates the patient’s heart and lung function to ensure they can withstand the surgery. Psychological evaluations help assess the patient’s mental health, ability to adhere to post-transplant care, and support system, which is critical for recovery.
Additionally, patients are educated about the transplant process, potential risks, and the need for lifelong medication adherence. This stage aims to ensure that the patient is a good candidate for transplant and can handle the demands of post-operative care.
Matching & Allocation Stage
Once a patient is deemed eligible for a liver transplant, they are placed on the national transplant waiting list. The matching and allocation stage involves finding a suitable donor liver for the recipient. Donor livers can come from deceased donors or, in some cases, living donors who donate a portion of their liver.
The matching process is based on several factors, including blood type, body size, the severity of the liver disease (measured by the MELD score, which stands for Model for End-stage Liver Disease), and geographic location.
When a compatible donor liver becomes available, the transplant team must quickly evaluate the donor organ’s suitability and condition. The patient is notified and prepared for surgery if the match is confirmed.
Surgery Stage
The surgery stage involves the actual transplant operation, a complex procedure typically lasting between 6 to 12 hours. The patient is placed under general anesthesia, and the surgical team begins by making an incision in the abdomen to access the liver. The diseased liver is carefully removed, and the donor liver is positioned in place.
The surgeon then attaches the donor liver to the patient’s blood vessels and bile ducts, ensuring proper blood flow and bile drainage. This step requires meticulous precision to ensure the new liver functions correctly and to minimize complications such as bleeding or bile leaks.
Post-surgery, the patient is transferred to the intensive care unit (ICU) for close monitoring. The initial days and weeks following the surgery are critical as the medical team watches for signs of organ rejection, infection, and other potential complications. Patients typically remain in the hospital for several weeks and require regular follow-up visits to monitor liver function and adjust medications.
Learning about the aspects of individuals who require liver transplantation helps to highlight the importance of early diagnosis and management of liver diseases. Timely intervention with liver transplantation can improve outcomes and provide a second chance at life for those suffering from severe liver conditions.
In conclusion, the liver transplant process involves a thorough evaluation to determine candidacy, a careful matching and allocation process to find a suitable donor, and a complex surgical procedure followed by intensive post-operative care. Each stage is vital to the transplant’s overall success and the recipient’s long-term health.