Toxic Agents To The Liver
Liver toxicity, caused by agents such as alcohol, acetaminophen, statins, and methotrexate, is a significant health risk if not properly managed.
Understanding the mechanisms by which these agents harm the liver, recognizing the associated risk factors, and identifying symptoms early can lead to effective diagnosis and treatment.
The following discusses the most common toxic agents to the liver and the treatment measures to manage this toxicity.
Common Toxic Agents
The liver functions to metabolize and detoxify substances that enter the body. However, specific agents can be particularly harmful to the liver, leading to liver damage or failure if not treated effectively. This section elaborates on four common agents known for their hepatotoxic potential: alcohol, Tylenol (acetaminophen), statins, and methotrexate, discussing their effects on the liver, associated risks, and important considerations.
1. Alcohol
Alcohol is one of the most well-known hepatotoxins. Chronic alcohol consumption can lead to a range of liver diseases, including fatty liver (steatosis), alcoholic hepatitis, fibrosis, and cirrhosis. Alcohol is metabolized in the liver by enzymes such as alcohol dehydrogenase and cytochrome P450 2E1, which produce acetaldehyde, a toxic metabolite that contributes to liver injury.
Risks
The risk of liver damage from alcohol is dose-dependent, with heavy and prolonged consumption significantly increasing the likelihood of liver disease. Factors such as genetic predisposition, gender, and coexisting liver conditions (e.g., hepatitis B or C) can also influence the severity of alcohol-induced liver damage.
Moderation in alcohol intake is the best way to maintain liver health. For men, moderate drinking is defined as up to two drinks per day, while for women, it is up to one drink per day. Complete abstinence is recommended for individuals with existing liver disease or those at high risk of developing liver problems.
2. Tylenol (Acetaminophen)
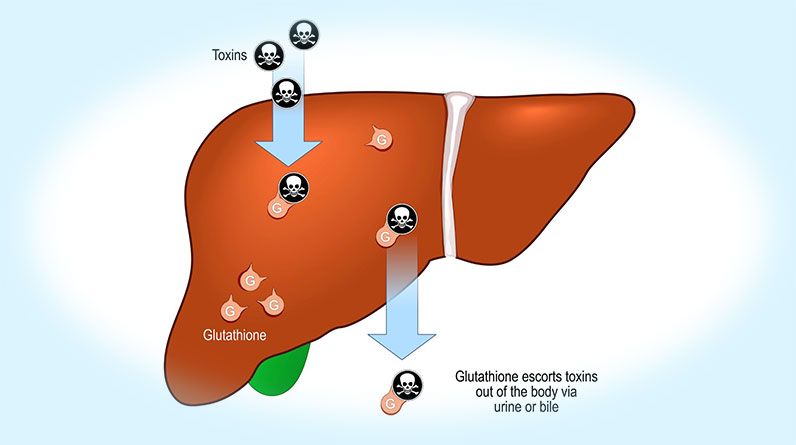
Acetaminophen, commonly known by the brand name Tylenol, is a widely used over-the-counter pain reliever and fever reducer. While safe at recommended doses, excessive intake can lead to severe liver damage. Acetaminophen is metabolized in the liver, and high doses can deplete glutathione, an important antioxidant, which leads to the accumulation of toxic metabolites that cause hepatocellular injury and necrosis.
Risks
The risk of liver damage from acetaminophen increases with doses exceeding 4,000 milligrams per day for adults. Accidental overdose often occurs due to the concurrent use of multiple medications containing acetaminophen. Liver toxicity is also heightened in individuals with chronic alcohol use or pre-existing liver conditions.
To minimize the risk of liver damage, it is essential to adhere to the recommended dosage guidelines for acetaminophen and avoid the simultaneous use of multiple acetaminophen-containing products. Patients with liver disease or those who consume alcohol regularly should consult healthcare providers before using acetaminophen.
3. Statins
Statins, such as atorvastatin and simvastatin, are commonly prescribed medications for lowering cholesterol levels to reduce the risk of cardiovascular diseases. Statins work by inhibiting the enzyme HMG-CoA reductase, which facilitates cholesterol synthesis. While generally safe, statins can occasionally cause liver enzyme elevations, indicating liver stress or damage.
Risks
Liver enzyme elevations due to statin use are usually mild and asymptomatic, occurring in about 1-3% of users. However, severe liver injury is rare. Risk factors for statin-induced hepatotoxicity include high doses, pre-existing liver disease, and interactions with other medications that affect liver metabolism.
Routine monitoring of liver enzymes before and during statin therapy is recommended to detect any potential liver issues early. Patients should report any symptoms such as fatigue, weakness, loss of appetite, abdominal pain, dark urine, or jaundice to their healthcare provider promptly.
4. Methotrexate
Methotrexate is a medication used to treat various conditions, including certain cancers, rheumatoid arthritis, and psoriasis. It works by inhibiting the enzyme dihydrofolate reductase, affecting DNA synthesis and cell replication. Methotrexate can cause liver damage through mechanisms such as oxidative stress, mitochondrial dysfunction, and direct hepatocyte toxicity.
Risks
Long-term use of methotrexate, especially at high doses, is associated with an increased risk of liver fibrosis and cirrhosis. Contributing risk factors include excessive alcohol consumption, obesity, diabetes, and pre-existing liver conditions. Regular liver function tests are necessary to monitor liver health in patients on methotrexate therapy.
To reduce the risk of liver toxicity, it is necessary to follow prescribed methotrexate dosages carefully and avoid alcohol. Regular monitoring through liver function tests and, in some cases, liver biopsies, is the way to prevent liver damage.
Diagnosis and Treatment
Diagnosing liver toxicity begins with a thorough medical history and physical examination to identify symptoms, medication usage, and potential exposure to hepatotoxic substances. Laboratory tests, including liver function tests (LFTs) and complete blood count (CBC), also help assess liver enzyme levels and signs of other damage.
Finally, imaging studies like ultrasound, CT scans, and MRIs provide detailed views of liver structure, while a liver biopsy may be necessary for a definitive diagnosis.
Treatment, on the other hand, focuses on stopping exposure to the toxic agent, such as discontinuing hepatotoxic medications or abstaining from alcohol. In cases of acute toxicity, interventions, like activated charcoal or N-acetylcysteine (NAC) for acetaminophen overdose, are appropriate methods for treatment.
Supportive care includes proper hydration, nutrition, and vitamin supplementation. Lifestyle changes, such as maintaining a healthy diet and monitoring liver function, are necessary for recovery.
Finally, in severe cases, advanced treatments like liver transplantation may be considered. Early detection and management lead to the best outcomes.
Through a combination of medical history and testing, healthcare providers can accurately diagnose liver toxicity and initiate appropriate interventions. Maintaining liver health involves adhering to medication guidelines, moderating alcohol consumption, and regular testing.